GASTRO COMMUNITY CENTER
Chronic functional digestive disorders and conditions affect over 68,000,000 Americans, yet there is little medical research and treatment for them and it is frustrating to see the lack of significant pharmaceutical advances that focus solely on treating a GI disease. Medications prescribed are often still considered experimental to a degree and patients are left exacerbated and disheartened by a vast and overwhelming medical system.
How can a service foster collaboration across medical fields and between patients to treat some of the most serious and underrepresented digestive diseases? How can we help patients feel connected and important as they’re guided and encouraged to make the drastic life changes required of their illness?
Using design and in-depth medical research to develop a more comprehensive healthcare facility, I proposed a service and space that will focus on creating tangible elements of the biopsychosocial therapy model to facilitate greater collaboration and multi-disciplinary input between medicine, nutritional science, psychology, and sociology. Patient teams will be prompted to treat on a community-driven and pro-active level that is less reductionistic and detached.
As the focus of my research thesis, I began to study some of the medical establishments that were at the forefront of healthcare design and looked to them as case studies for user experience and service design. I also looked to experimental food labs and researched diagnostic procedures, treatments, and medications. What were the experiences people were going through on their medical journey to diagnose and treat these disorders? Were these treatments working? What was missing?
Aside from the physical space, I wanted to disrupt the entire facility model and our perception of a healthcare center. The more I spoke to peers and held discussions with members on online support groups, I realized there was a crucial gap in addressing the psychological aspect of patients' journeys. Many gastrointestinal disorders are difficult to diagnose and patients often feel isolated, like they're suffering silently while appearing healthy on the outside. I then studied the effect that habitual stress has on the body and nutrient absorption, an already pressing issue with these disorders.
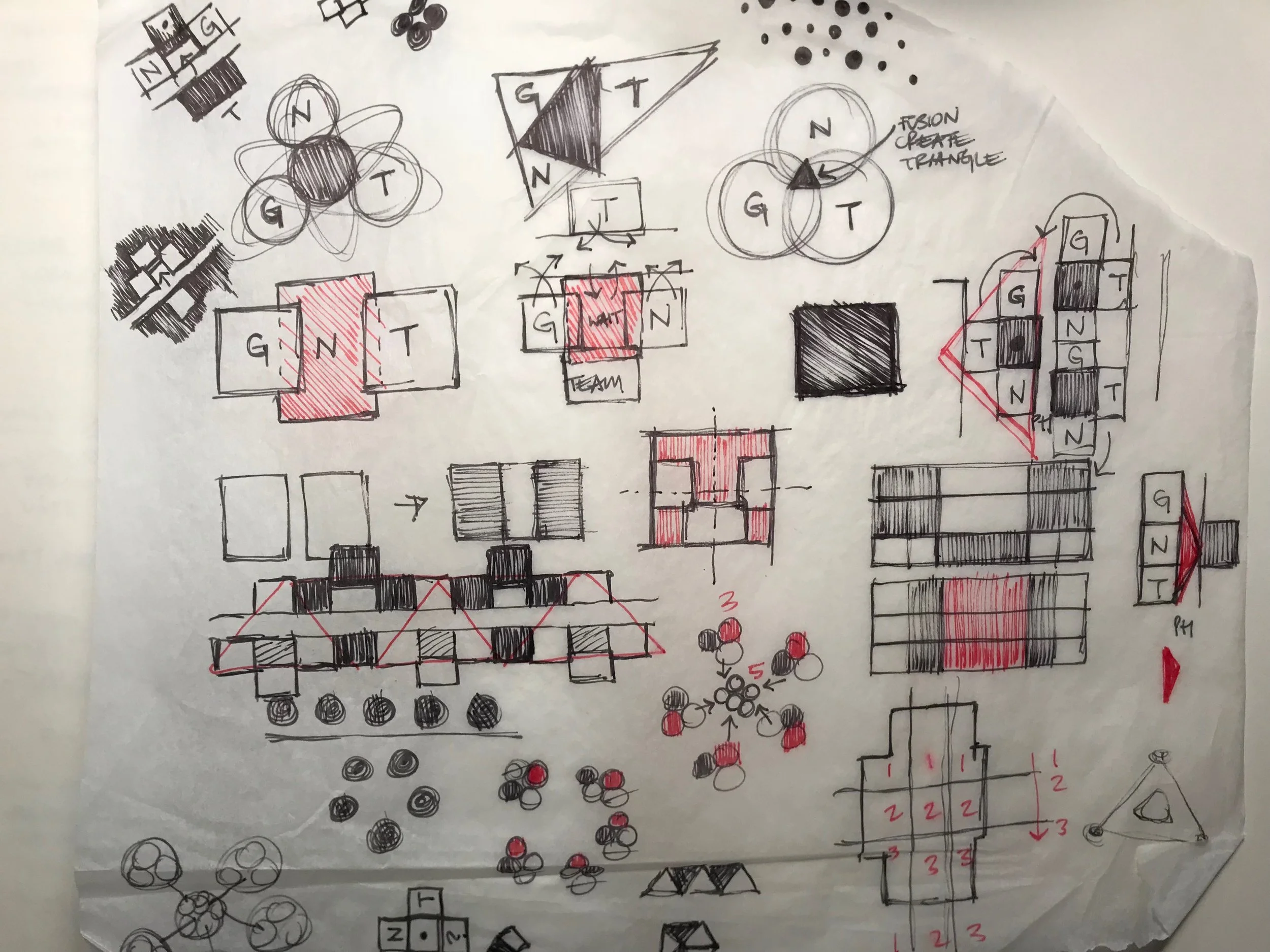
With that, I shook up my original patient team model of gastroenterologist/dietician and created one that was even more interdisciplinary. One that addressed patients needs from greater angles and also I considered levels of communication throughout the center between various disciplines and staff members.
I planned for vertically integrated features to the center that would engage patients, draw in the community, and support back-door functionality. Throughout the process, the experience of a diverse range of patients was considered paramount, from pediatrics through bariatric care, in addition to work flow for staff.
However, as any good designer knows, the first main task in applying this research was to study adjacencies, program requirements, and outside factors (such as light, privacy, and sound) prior to blocking out and testing various frameworks and plans for the most-efficient and user-friendly design.
THE FINISHED PRODUCT
The result was the GCC, a hybrid medical community center. In an effort to provide ongoing service in support of the patient's journey, patients could receive medical procedures and therapy sessions, but also partake in therapeutic learning activities with the greater community from cooking in the test labs, connecting in the cafe, or gardening on the green roof with medicinal herbs that aid in digestion.
A full copy of the research portion has been added below.
Happy reading!